Last week I had the huge privilege of being invited to give a keynote speech at this year’s Auspath (Australian association of transgender health) conference, held in Tasmania. I loved being at Auspath, met many awesome people, and enjoyed learning about Australian approaches and best practices, many of which I wish the UK would learn from. There were also a couple of things at Auspath that gave me pause. In this blog I’m going to briefly run through some of the things I liked best at Auspath, before a deeper dive into two areas of that left me thinking. I don’t claim to have all the answers, but am sharing my current thinking – I would love to hear other people’s takes, on their experience at Auspath, on their priorities for improving trans youth healthcare in Australia and beyond, and on their experience and perspectives on the two issues covered at the end of this blog.
Highlights
It was a rare joy to be around so many incredible people fighting hard for a positive future for trans kids. I really valued:
- Hearing so many clinicians speaking with genuine compassion and respect about trans lives. Even where I took issue with a minority of clinical approaches, the professionals I heard at Auspath clearly cared for trans youth, clearly had a base level of respect for trans lives, clearly wanted the best. It is a very different world from the UK where I can count on one hand the number of NHS professionals I’ve met who I’ve heard speak respectfully about trans kids. I’ve focused the latter sections of this blog on critique rather than praise, because pretty good shouldn’t be the bar – Australia has the potential to be world leading in trans youth healthcare.
- Hearing so many professionals, advocates, community members, parents, allies, speaking with determination about protecting trans kids and trans healthcare from the abuses spreading across the world.
- Hearing an impressive and eloquent young person speak about their experiences, including obstacles and barriers to equal access to healthcare.
- Hearing an impressive and eloquent parent share their experience on the difficult path advocating for a trans child in Australia.
- Learning about Country and first people’s knowledge and experience. It would have been good to hear more on the topic of first people’s experiences and priorities.
- Listening to a panel talk about the fight for trans kids in Queensland (I was crying through most of that panel).
- Feeling really welcomed at the conference, some many people came up to me with kind and friendly words, and I also felt very welcomed as a non-binary person in that space.
- Hearing a panel of young adults speak on their experience advising on trans health research projects, on the need to include young people who were unable to access paediatric services, the need to include rural youth, the need for fair pay, for both career development opportunities for those who are research inclined as well as keeping space for input from young people with no interest in working in research. The importance of disability justice informed approaches.
- Meeting young adults who are willing to challenge establishment status quo approaches. I think this is really valuable. So much cis-supremacy and cisnormativity operates through the maintenance of outdated systems and approach that we don’t even question. Having young people speak up and ask these questions is super important. One such question was ‘do we ever need to collect and report on data on assigned sex/gender?’. It’s a really good question. My current answer is ‘I don’t know, but certainly very significantly less than we do at present. This is definitely a question I will carry with me. I’m doing a new piece of research at the moment on non-binary adults and in that survey we are including a specific question ‘do you want to see results from this research broken down by assigned sex/gender?’, along with open text boxes for people to share their reason for or against. These answers should likely be context specific and driven by the information needs of the people whose data it is. Certainly we should have already moved away from the approach I still saw some places in Auspath where a person was introduced as ‘patient A – AFAB – identifies as a boy’.
- Meeting lots of awesome people from New Zealand, commiserating and strategizing on how to fight and support young people through state enforced discrimination.
- Meeting lots of healthcare providers working outside of specialist gender clinics, who are working to develop alternative routes to respectful and informed consent care. Many of these are currently supporting adults – with confidence and advice the same care can be extended to under 18s.
There were two points in Auspath where I heard completely different messages from different people, and that relates to the two topics that I’d like to do a deeper dive into in this blog: MDT assessment and comprehensive bio-psychosocial assessment. Some people came up to me and expressed concern that such things were happening in the UK, and that we should fight them being introduced in Australia. Other people came up to me to share their knowledge of these practices being experienced by trans children in Australia.
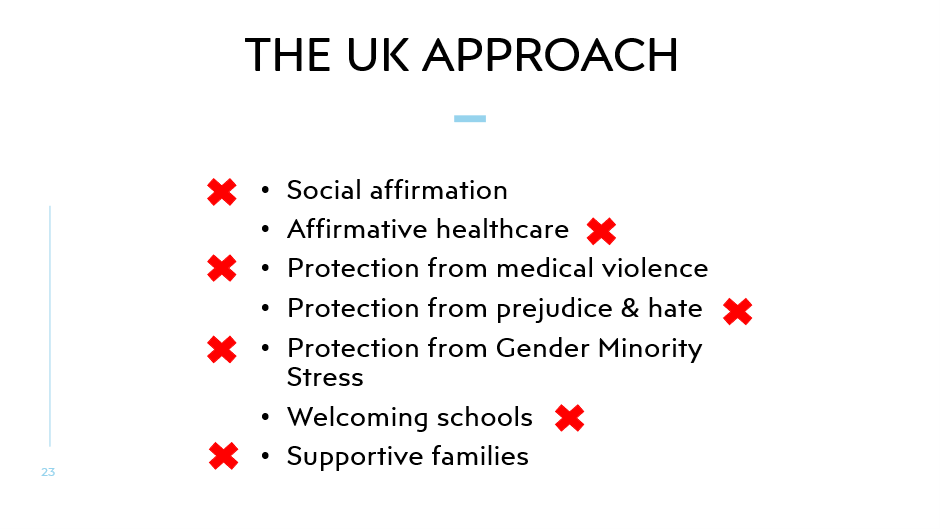
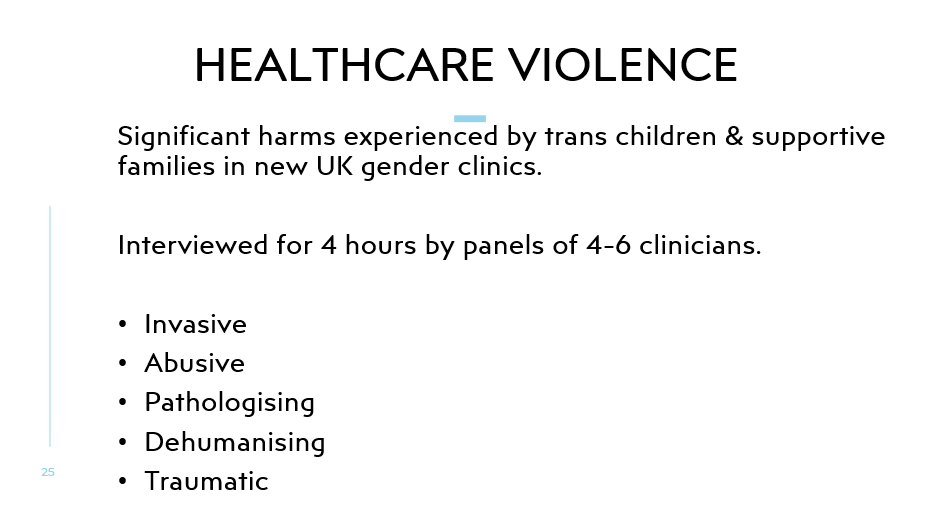
In my presentation I spoke about the harms of excessive questioning of trans kids. In the UK this 100% comes from a position of bad faith. Clinicians are encouraged to ask hundreds of questions, with an intention of probing, prodding and undermining trans identities. At Auspath I did not hear any explicitly and intentionally bad faith or actively transphobic intent. I did however, from some clinicians, hear approaches that, whilst coming from a better place, constitute the same excessive questioning. In Australia this excessive questioning was sometimes marketed and justified as ‘adding value’. Even from some brief conversations with service users I heard people share stories of having experienced this ‘added value’ as harmful. I would really like to call attention to the over questioning of trans kids even in nominally affirmative services. Being trans is normal, and trans kids shouldn’t be faced with extensive additional healthcare questioning compared to their cis peers. Any systems that normalise asking additional bio-psycho-social questions of trans kids compared to what is standard for cis kids is a problem. And here, our base comparator should not be the among of questioning that is standard for cis kids who need psychiatrist or psychologist support – our comparator should be an average cis kid who is not under psychologist or psychiatrist led care. Simply being trans, or accessing trans healthcare, does not justify invasive and excessive psychology centred questioning – this approach is a legacy of pathologisation. Two phrases were heard at Auspath more than I would like: Multi-Disciplinary Team Assessment, and Comprehensive Bio-Psycho-Social Assessment.
Multi-Disciplinary Team Assessment
In the UK it is presumed that a trans child needs to be assessed by multiple different professionals, often including a psychologist, psychiatrist, paediatrician, social worker, and that is before assessments with an endocrinologist or fertility specialist. These multiple levels of assessment are abusive and excessive. At Auspath clinicians listed a dizzying array of different professionals being involved in MDT assessment of trans kids. In Spain, in the highly respected Transit service in Catalonia, trans kids see one medical professional, usually a GP. The GPs role is to support informed decision making by a trans young person (and their family depending on age), their role is not to assess and decide upon access to healthcare. In this Spanish service that one medical professional, that one GP, can provide healthcare, including endocrine care for trans adolescents, without input from additional professionals. They do still operate in what they describe as a multidisciplinary team, having different colleagues within their service. This multidisciplinary team allows the GP to offer access to different additional services, optionally, in an opt-in approach. Young people can ask to additionally see a psychologist. They can ask to see a social worker or family worker, to support with school for example. But these additional professionals are additional optional services, a trans young person does not have to see, and certainly does not have to be assessed by, a whole multidisciplinary team of different professionals.
At times in Australia it was unclear to me what different clinicians mean when they refer to multi-disciplinary team working. I hope Australian colleagues can consider and articulate where they are working within an MDT that offers optional opt-in access to a range of different professionals, without mandating that a trans child see an overwhelming range of different professionals. I hope clinicians can be clearer in whether their approach forces trans young people into running a gauntlet of different stages of assessment by a series of different professionals. I hope more attention can be drawn to the harms of forcing trans children through multi-professional assessments where additional professionals are not desired or needed. WPATH SOC 8 recommends an MDT assessment for trans adolescents – I hope Australia can be part of building an evidence base for a better approach in time for SOC9.
Comprehensive Bio-Psycho-Social Assessment.
This is a term that I find really triggering. In the UK this term is used to define practices that are pathologising, intrusive, uncomfortable, and harmful for a trans child. When I first heard this term from clinicians in Australia I assumed it meant something else here. I initially hoped that it was being used as a defensive practice, by clinicians under anti-trans pressure, who are keen to emphasise the thoroughness of their care, using this term as a fancy descriptor for actions that I, as a non-clinician, would describe as ‘having a chat’, or ‘getting to know your patient’. A good GP can ‘have a chat’ with a patient, and quickly find out some useful information about them to better help them understand, build rapport with, and support their patient. This can include some brief questions to understand their life circumstance, their family support, their strengths, supports, stresses or concerns. This can be done rapidly in a first appointment as a non-intrusive, flexible, patient-centred and low stakes chat. This should not be defined as a ‘comprehensive bio-psycho-social assessment’.
I was chatting to one clinician, who described taking notes during such a ‘getting to know you’ chat, with those notes not affecting care pathways but being taken primarily to enable quicker rapport building at the next appointment. I commented that I find it really uncomfortable to have clinicians take notes when I am asked questions about my life and circumstance. This is clearly linked to my own institutional trauma in unsafe healthcare settings where answers to these questions are definitely being judged by clinicians, where answers might end up in a non-consensual case study report, and where these notes do impact on your (or your child’s) access to care. It is important for good healthcare professionals to note how much institutional trauma and distrust many trans people, including trans kids, carry into the clinic. Even young people I met in Australia spoke at length of trauma experienced in encounters with various healthcare professionals who were there to judge and control.
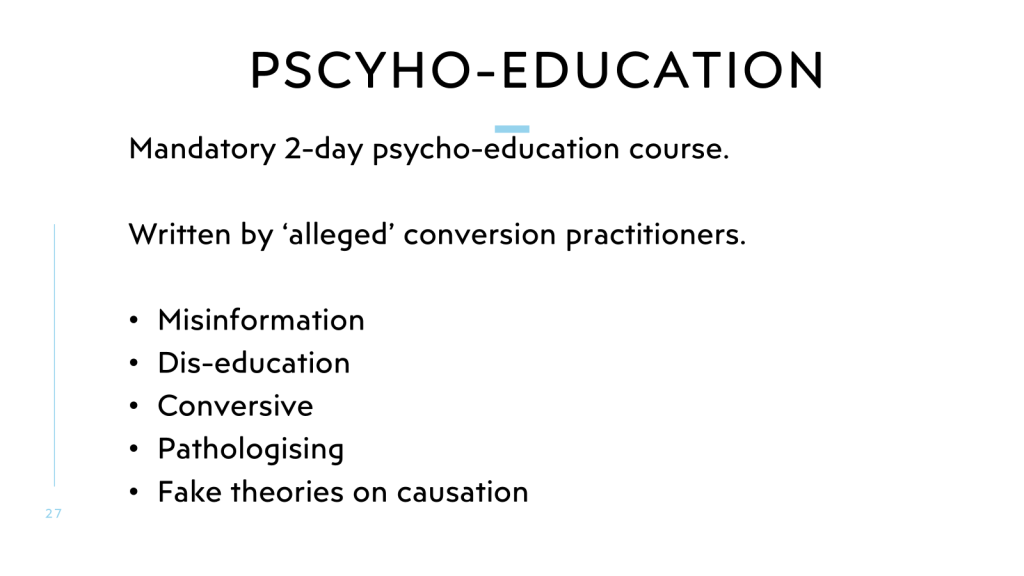
I had initially hoped that references to ‘comprehensive bio-psycho-social assessment’ were just a sign of defensive practice. I was dismayed and at one point upset to hear that actual comprehensive bio-psycho-social assessments are still a core part of care in locations across Australia, particularly in trans children’s healthcare, particularly in services delivered by mental health professionals. I was disappointed to see reference to incredibly detailed family tree mapping, filled with details entirely unrelated to a child’s access to trans healthcare services. I was disappointed to see wide-ranging body mapping exercises, children asked to draw themselves, notes taken on left or right handedness, even assessments of pen grip. Many of these unnecessary and pathologising over-assessments were marketed and justified by professionals as ‘adding value’. If we are seeing a trans kids, we ‘might as well’ assess whether they are having trouble holding a pen. We might as well investigate their full family system for areas of family disfunction. We might as well screen for ADHD, autism, anxiety, anger issues, dyslexia, poor family functioning, disordered eating, sexual health support needs, bullying support needs etc etc.
The list of things we ‘might as well offer’ as ‘added value’ while we are here grows ever longer, especially in trans children’s healthcare. Some of this emphasis on ‘added value’ is perhaps a symptom of some professionals realising that the original reason for their role is outdated, pathologising and unneeded. But why are ‘added value’ assessments brought into trans children’s healthcare? Why are trans children’s healthcare assessments so broad, ill-defined, all encompassing? The answer lies in services that are struggling to adapt from a pathologising model of care.
In terms of unnecessary questioning added on to trans healthcare, I am perhaps least worried about short screening questions that are designed to triage young people to additional support services that might well be beneficial. Some trans kids might also want an ADHD assessment. Some might want support for anxiety. But even then I’d rather this was done transparently, optionally, and with patient consent ‘would you like to do a few additional questions to help us see whether you might benefit from our optional mental health or neurodivergence services including related to anxiety, ADHD, eating disorders etc. For triaging child developmental concern, this can be similar ‘while you are here, would you like us to check your/your child’s pen grip, for dyslexia etc’. This transparency is important as it helps service users understand and have trust in the process, while also letting them tell clinicians when ‘added value’ services are not need, are already being managed by other professionals or are not wanted at this specific time. Crowding all types of assessment into a trans health assessment makes these extra long and stressful.
Then there are areas of a comprehensive bio-psycho social assessment that are clear remnants of past pathologising models. Questions on childhood toys, friendships, family gender roles, sexuality of parent or child, and many other unnecessary questions are inappropriate. At the conference there was one exchange that was particularly noteworthy. A clinician commented that they always ask trans young people about their romantic relationships. They noted that young people commonly respond by querying ‘why are you asking this?’. They said that they then tend to respond ‘Because it helps remind me that you are a full human, more than just your gender/transness’ (I didn’t take live notes and won’t be getting the statement 100% accurate).
I had three reflections on this answer. Firstly, it is important to recognise power dynamics in a clinical encounter. It is hard for any service user to question the approach of their clinician. It is particularly hard in a trans healthcare appointment, and especially so for a child. If young people are questioning our approaches, we would do well to take this as a significant potential indicator of discomfort. It is really hard for a child to question an authority figure, especially one whose approval they need. If we are asking questions that young people indicate some level of discomfort with, if there is not a very strong clinical need, surely we should not be asking those questions.
Secondly, I note that the young person’s question ‘why are you asking this’ was not provided a satisfactory answer. Clincians should not need private information on trans people’s lives in order to remember that we are more than being trans. I don’t think the speaker realised the impact of their words on some trans people in that room. I left the room at that point. There is a long history of trans people, especially trans kids, being asked invasive questions for no reason other than to satisfy clinician curiosity. Curiosity driven questions are entirely inappropriate – we shouldn’t have to humanise ourselves in order to access healthcare.
Thirdly, sexual orientation and relationships questions are often asked without clear purpose. In the UK these questions are deemed necessary based on anti-trans fake theories of childhood transness being a reaction to homophobia or sexual abuse. In the UK’s puberty blocker trial these are also justified through inclusion of a criteria excluding youth with any judged potential for having unprotected sex from eligibility to access the trial.
In less transphobic services these questions are sometimes justified by reference to a need to screen for unmet sexual and reproductive health information and support needs. I would tend to agree that trans youth may have unmet sexual and reproductive health information and support needs. Schools, regular resources and parents may all be ill-equipped to provide trans-inclusive education. But screening for unmet sexual and reproductive health needs can be done transparently, intentionally, none creepily and with consent. It does not need to be untransparently sneaked into a wider trans healthcare assessment, where historically youth have been forced to answer unwanted and intrusive sexual questions driven by clinician curiosity or clinician ignorance, unrelated to screening for sexual and reproductive health services. I would suggest that asking a young trans adolescents about their sexual and romantic relationships or desires is rarely an effective strategy in building rapport. When asking potentially irrelevant questions that are likely to make a young person uncomfortable it is not sufficient to give them an option not to answer. Some questions should not be asked. I’ve accessed specific sexual and reproductive health services as an adult without being asked any of the type of personal questions that psychologists and psychiatrists sometimes feel entitled to ask of trans children.
I would strongly question the appropriateness of insisting on a comprehensive biopsychosocial assessment in trans youth healthcare. I would ask clinicians to document much more clearly the questions they are asking and the purpose or clinical need for each question. I would suggest tat rapport building questions should be short, comfortable, flexible and non-intrusive. I would suggest that ‘added-value’ screening questions to triage to additional support services should be transparent, opt-in areas of questioning, strongly delineated from what is being assessed.
I hope we can quickly evolve away from assessment-based models of care for trans children and young people. And while assessment remains, we all have a shared duty of care to reduce the exceptionally excessive breadth and depth of questions that have become wrapped up in a comprehensive biopsychosocial assessment. Professionals who are able to deliver effective rights-respecting healthcare to trans children and young people in Australia without invasive psychological and psychiatric assessment as standard, please can you more clearly communicate what questions are actually clinically necessary, whilst also documenting the questions that you consider not clinically valid. (I’m happy to anonymously share examples on my blog).
Trans healthcare is not a psychological or psychiatric treatment, and we need to move trans children significantly further from being in positions of psychology/psychiatry-centred questioning and assessment. I’m not against jobs for psychologists and psychiatrists – we can channel those existing resources into helping trans kids with anxiety and stress related to living in a trans-hostile world, and into treating the adults around them who fall into anti-trans radicalisation. Trans kids in rights-respecting healthcare services across different parts of the world receive trans healthcare without a comprehensive biopsychosocial assessment, and we can aspire to this across Australia.
Flight home
After Auspath I tagged on a few holiday days in Tasmania, seeing some beautiful landscapes and wildlife, an incredible experience. I’m writing this blog whilst rather sleep deprived and time-zone confused on a long flight back to the UK. In the two weeks I was away, the UK has completely removed protection for non-binary people (in a legal case that made absolutely no sense); the UK has banned trans girls (and trans women as leaders) from girl guides; and banned trans women from the Women’s Institute. These are all severe blows. Girl Guides has long been one of the best allies for trans girls – an organisation whose inclusive policy we have long pointed to when asking for schools or other organisations to choose equality and inclusion. Having them bow to transphobic pressure is a blow not only for the impact on Girl Guides, but for what this means for the whole state of inclusion of trans girls in UK society.
I have felt so much lighter and safer being in Australia and fly ‘home’ with significant trepidation and fear for the future. At least I am re-energised from feeling safe and hopeful through my days in Australia and at Auspath. But the fight goes on.
Thanks to anyone who got to the end of a very long blog!
In cross-national solidarity,
Cal